EU Healthcare Interoperability Standards
Published : Tuesday 11 December 2018
Timely and unhindered access to health records in a portable format should be a fundamental right for all citizens ...

Please note: this content is 7 years old. It may be of lower quality or no longer accurate.
Our health and wellbeing can be impacted by the availability and integrity of our medical records and we may come to harm or even die due to the right information not being available at the right time. Therefore globally, we must move to a position where the citizen’s right to timely and unhindered access to their health record in a portable format is a fundamental right for all citizens.
This issue is particularly key when healthcare spans multiple organisations, regions and indeed countries, making the portability of data critical to safe, efficient and effective healthcare. This is particularly true in Europe where the free flow of data is necessary to underpin Directive 2011/24/EU, an EU citizens’ right to cross-border healthcare.
As an EU citizen (at least for now if you are British), the directive gives us the right to be treated by public or private healthcare providers in the EU and makes prior authorisation for cross border care the exception rather than the rule. Whilst there are many issues surrounding this long-standing directive, not least the willingness of some governments and health systems to honour citizens’ rights, the flow of data is obviously one of the key enablers.
The EU Commission recently announced a proposal which will make recommendations on how electronic health records can be accessed and shared more easily in every EU member country.
The idea being that it will make it easier for patients and the wider health eco-system, to use health information across the EU – which will lead to safer and more effective care, not only across Europe but within member states where data portability issues often plague healthcare delivery.
However, there are wider issues to consider beyond data standards alone, and indeed just the notion of standards may well be part of the problem, or more specifically the standards “debate”.
At the highest level, key to enabling cross border care is to give citizens greater agency, after-all, the individual is the only one who truly understands their relationships with all their healthcare providers.
Therefore, it follows that the individual is in an ideal position to aggregate a complete and longitudinal record when given the appropriate means to do so.
This is especially true when considering healthcare systems such as the NHS. The NHS has spent tens of years and as many £billions taking an organisational approach with limited success, whilst at the same time denying patients agency and choice - this is bad for everyone.
The landscape today
Within healthcare today there exist many technical capabilities which would enable the first step towards giving agency to patients, including patient facing portals and downloads. Going beyond this the ability for the patient to mobilise their data securely requires APIs (Application programming interfaces) which are digital interfaces to allow data to be transferred between systems. With the right approach this can be done at the discretion of patients.
In healthcare we hear of the lack of capabilities and problems with suppliers, however the core technical means are often already in place. For example, major systems such as Epic, Cerner, Allscripts, and even in local systems with a great deal of legacy already have a great deal of support for patient facing services.
Indeed in the US, regulation has required healthcare providers to expose such capabilities over the years. More recently this mandate has been extended to APIs, and we are now starting to see APIs publicly exposed to patients and standards such as HL7 FHIR being adopted.
So at least for the basic information flows the technology and standards are not necessarily the issue.
What’s the real issue?
Perhaps the main issue with medical record access is not one of technology but one of people, politics and process.
Attitudes and cultures vary significantly across countries with some seeing the solution as being organisational silos and controlling everything from the provider (such as in the UK and Norway). Others (such as the Netherlands) are already more accepting of the need for patients and their data to move across borders, and now they just need the effective systems and processes to enable this.
It’s important to note that the majority of objections to patients having their health data have already been addressed by various projects, notably by the US Open Notes programme which has produced a wealth of evidence and tackled some of the most challenging areas, including mental health.
That said there are still organisations which continue to resist patients rights, and regulators have often been weak in enforcing these long standing arrangements such as the UK 1998 Data Protection Act.
Even where organisations do move forward they often fail to learn from other health economies and sectors, continuously re-inventing and piloting, suffering from a severe case of “not invented here syndrome”.
What is needed is for the commission to make clear that the regulatory frameworks are in place and demonstrate that these are enablers to empowering citizens and not barriers.
Regulatory capture
One key issue most health economies face is the vested interests of various parties and what some have described as anti-competitive behaviour. Indeed in senior ranks these issues are often discussed around the water-cooler but little or no action has been brought to bear by those in authority.
Perhaps most frustratingly, where there is a vested interest in the data flowing, data is actually shared, usually for secondary purposes. For example:
- US health data flows to support payments and insurance claims.
- NHS patients data is regularly used for secondary purposes such as reporting and invoicing.
- More recently the NHS (unlawfully) shared 1.6 million patient records with Google DeepMind, for commercial gain the details of which it has refused to disclose to patients.
From system suppliers trying to protect and extend their market share, to healthcare providers building their empires and their cottage industries, there are many non-technical reasons which stand in the way, and all too often it is patient who suffers as a result.
The “standards” debate and the subsequent technical requirements, contracts and importantly who will pay for all of this is an ideal vehicle for those with vested interest in delaying progress and creating “jobs for the boys” within the technology community and cottage industries.
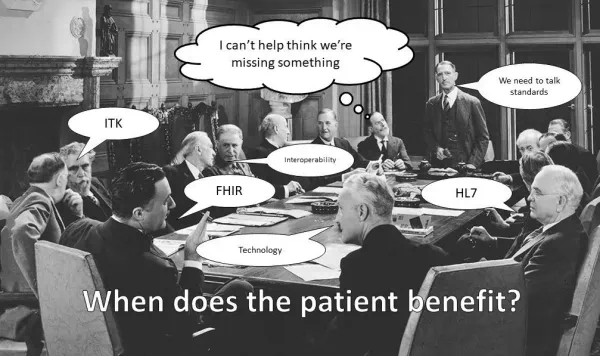
(Click for full resolution)
Silo mentality
Healthcare has a long history of trying to integrate systems and on the whole had limited success due to the broad and complex nature of healthcare services, systems, data and the inability to escape what is essentially a complex mesh network.
Caution should also be exercised when it comes to institutional interoperability, as this does not address the issue of data portability and has proven complex, costly and yielded very limited results.
For example the NHS has spent many years and £10’s billion and yet still, data generally remains in silos, inaccessible across providers and incredibly hard / burdensome for patients to access.
Exposing portals to patients has certainly offered some benefits, but on the whole their availability is generally poor and the utility they provide, in particular when it comes to pathway specific support is poor and therefore uptake can be low.
This low uptake is sometime misconstrued as patients not wanting their data, when in reality many patients do, but the systems and services of today do not given them utility or the ability for patients to reuse their data in a manner which suits as their particular needs.
A portal will never be all things to all people, therefore the key messages for healthcare providers are:
- Traditional point-to-point interoperability and more silos are not the solution.
- The solution is opening up data and enabling portability so that patients can share and reuse their data on their terms.
By adopting this approach healthcare can enable data sharing across traditional boundaries, including countries, as well as enabling patients to meaningfully reuse their data for their care as well as with applications and services they choose.
The way forward
While it is hard to disagree we should all be working toward standards, most systems today support patient facing APIs and the key is to open these up immediately and work towards standards longer term.
This enables innovators and industry to get to work, while giving patients a greater agency from day one. Too much time has already been lost to the eternal standards debate.
The real world deployment of technology must take an agile and iterative approach, which focuses on low complexity high value quick wins. For example, the sharing of basic information types (such as medications, conditions, allergies, observations, immunisations and encounters) while working towards more complex types such as documents and imaging data.
It is important to stress that the agile approach must be applied to the adoption of technology, not simply the development cycle, otherwise we see long periods of design and development with no real world benefit.
Another key point to consider is the enormous amount of time lost to trying to specify coding schemes and standards. What many patients need is information such as what, when, where and by who.
Using common standards should be encouraged but not to the detriment of progress, especially when simply documenting and publishing what is already available will provide incredible mileage. You can bet Google didn’t sit down with British Gas and pore over standards, and yet your boiler can talk to your Google Calendar to know your schedule.
The public publication of documentation and API endpoints is increasingly commonplace in the US, but in health economies such as the NHS many of these are hard to come by and ludicrously some even sit behind none disclosure agreements. There are no good reasons for this.
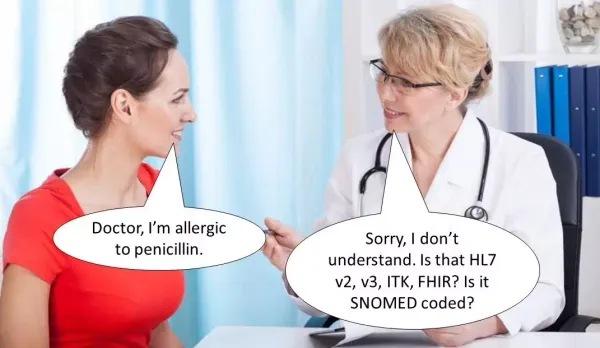
(Click for full resolution)
What should we ask of the EU Commission?
In order to move the health information sharing agenda forward, patients need the EU to consider issues wider than just standards if we are to truly enable cross border information sharing :
- Reaffirm the rights of citizens to choose their healthcare provider and ensure member states honour this.
- When it comes to medical records themselves, it is critical the EU emphasise the rights of citizens and ensure member states honour and police these effectively.
- Reinforce the message that we already have the technical capabilities today and regardless of standards, best practice is to make these available to patients now.
- Create a framework for healthcare providers to operate in and work towards regulation which enforces citizens rights to their data including APIs as in the US.
- Create a working party to shape standards and to help organisations go on the journey from open non-standardised systems, to standards based systems, in a truly agile and iterative manner.
Have your say
You can have your say on the EU Commission’s proposal on how electronic health records can be accessed and shared until the 20th December.
- EU Electronic health records standards
https://ec.europa.eu/info/law/better-regulation/initiatives/ares-2018-5986687
Useful links and references
- EU Cross-border healthcare
https://ec.europa.eu/health/cross_border_care/overview_en - US Open Notes Programme
https://www.opennotes.org - HL7 FHIR
https://www.hl7.org/fhir/
Dan's Blog
Information Technology, programming, health, fitness and photography enthusiast.
- Not a writer.
- All views are my own.
- Offence is optional.
- Do your own research.